Type 2 diabetes is a chronic condition that affects millions of people worldwide. It is characterized by insulin resistance and high blood sugar levels, often resulting from a combination of genetic and lifestyle factors. The question many patients and healthcare professionals grapple with is: Can you reverse type 2 diabetes? This article aims to delve into this question, exploring the scientific evidence, methods, and considerations for potentially reversing this condition.
Understanding Type 2 Diabetes
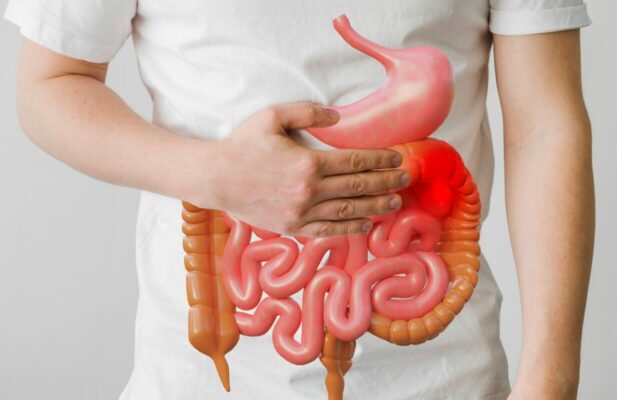
Type 2 diabetes occurs when the body becomes resistant to insulin or when the pancreas fails to produce enough insulin. Insulin is a hormone that helps glucose enter the cells to be used for energy. When this process is disrupted, glucose accumulates in the bloodstream, leading to high blood sugar levels. Over time, this can cause severe complications, including heart disease, kidney failure, and neuropathy.
Key Factors in Type 2 Diabetes
- Insulin Resistance: The body’s cells become less responsive to insulin, requiring more insulin to achieve the same effect.
- Beta-Cell Dysfunction: The pancreas’ insulin-producing cells fail to produce enough insulin in response to blood sugar levels.
- Genetic Predisposition: Family history and genetics play a significant role in an individual’s risk of developing type 2 diabetes.
- Lifestyle Factors: Poor diet, lack of physical activity, obesity, and stress are major contributors to the onset and progression of type 2 diabetes.
Can Type 2 Diabetes Be Reversed?
The concept of reversing type 2 diabetes is gaining traction among researchers and clinicians. While the term “reversal” implies a permanent return to normal glucose regulation without medication, it is often more realistic to aim for “remission.” Remission means maintaining blood sugar levels within the normal range without the need for diabetes medications.
Scientific Evidence for Reversing Type 2 Diabetes
Several studies have demonstrated that type 2 diabetes can indeed be reversed or brought into remission through various interventions, particularly lifestyle changes. Key findings include:
- Weight Loss: Significant weight loss has been shown to improve insulin sensitivity and beta-cell function. The Diabetes Remission Clinical Trial (DiRECT) found that nearly half of the participants who achieved weight loss of 10-15 kg were able to achieve remission of their diabetes.
- Dietary Changes: Low-calorie, low-carbohydrate, and plant-based diets have been effective in lowering blood sugar levels and improving insulin sensitivity. The Mediterranean diet, for instance, has shown positive results in managing blood sugar and reducing cardiovascular risk.
- Physical Activity: Regular exercise helps to increase insulin sensitivity and glucose uptake by the muscles. Both aerobic exercise and resistance training are beneficial in managing type 2 diabetes.
- Bariatric Surgery: For some individuals, surgical interventions such as gastric bypass or sleeve gastrectomy can lead to significant weight loss and improved glucose metabolism, often resulting in diabetes remission.
How to Reverse Type 2 Diabetes
Reversing type 2 diabetes requires a comprehensive and personalized approach. Here are the key strategies:
1. Weight Management
Achieving and maintaining a healthy weight is crucial. Weight loss helps to reduce insulin resistance and can restore the function of insulin-producing cells in the pancreas. Strategies include:
- Caloric Restriction: Reducing daily calorie intake can lead to weight loss. This can be achieved through portion control, choosing nutrient-dense foods, and avoiding high-calorie, low-nutrient foods.
- Meal Replacement Plans: Structured meal replacement plans, such as those used in the DiRECT study, can help individuals achieve significant weight loss and diabetes remission.
- Behavioral Therapy: Working with a dietitian or psychologist can help address emotional eating, establish healthy eating patterns, and maintain long-term weight loss.
2. Dietary Modifications
Adopting a healthy eating plan is essential for managing blood sugar levels and promoting weight loss. Effective dietary strategies include:
- Low-Carbohydrate Diets: Reducing carbohydrate intake can help to lower blood sugar levels and improve insulin sensitivity. Diets such as the ketogenic diet have shown promise in managing diabetes.
- Plant-Based Diets: Diets rich in fruits, vegetables, whole grains, and legumes have been associated with improved insulin sensitivity and lower risk of diabetes complications.
- Mediterranean Diet: This diet emphasizes healthy fats (such as olive oil), lean proteins (such as fish and poultry), and a high intake of fruits and vegetables. It has been linked to better blood sugar control and reduced cardiovascular risk.
3. Physical Activity
Regular physical activity is vital for improving insulin sensitivity and overall health. Recommendations include:
- Aerobic Exercise: Activities such as walking, running, cycling, and swimming can help to lower blood sugar levels and improve cardiovascular health.
- Resistance Training: Strength training exercises, such as weightlifting, can increase muscle mass, which helps to improve glucose uptake and insulin sensitivity.
- Consistency: Aim for at least 150 minutes of moderate-intensity aerobic activity per week, along with muscle-strengthening activities on two or more days per week.
4. Medical Interventions
In some cases, medical or surgical interventions may be necessary to achieve significant weight loss and improve glucose control:
- Medications: Some medications can aid in weight loss and improve blood sugar control. These include GLP-1 receptor agonists and SGLT2 inhibitors.
- Bariatric Surgery: For individuals with severe obesity, bariatric surgery can be an effective option for achieving long-term weight loss and diabetes remission. Procedures such as gastric bypass and sleeve gastrectomy have shown significant benefits.

Advanced Diabetes Solutions by Dr. Jonathan Spages
As a specialist in reversing type 2 diabetes naturally without drugs, Dr. Jonathan Spages offers advanced strategies that focus on holistic and integrative approaches. These methods aim to defy the odds and achieve diabetes reversal through natural means. Here are some key elements of Dr. Spages’ approach:
Personalized Nutrition Plans
Dr. Spages emphasizes the importance of personalized nutrition plans tailored to individual needs. These plans typically focus on:
- Anti-Inflammatory Foods: Incorporating foods that reduce inflammation can improve insulin sensitivity and overall health. This includes leafy greens, berries, nuts, seeds, and fatty fish.
- Glycemic Control: Selecting foods with a low glycemic index to maintain stable blood sugar levels. This involves minimizing refined carbohydrates and sugars.
- Nutrient-Rich Foods: Ensuring adequate intake of essential nutrients, such as vitamins, minerals, and antioxidants, to support metabolic health.
Functional Medicine Approaches
Functional medicine looks at the root causes of diabetes rather than just treating symptoms. Dr. Spages’ approach includes:
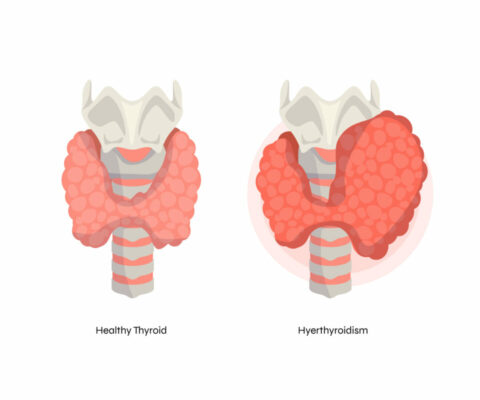
- Comprehensive Testing: Utilizing advanced lab tests to assess hormone levels, gut health, and other factors that may contribute to diabetes.
- Targeted Supplementation: Recommending specific supplements to address deficiencies and support metabolic functions. This may include omega-3 fatty acids, magnesium, and vitamin D.
- Detoxification Programs: Implementing detoxification protocols to reduce the body’s toxic load, which can impair insulin sensitivity and metabolic health.
Mind-Body Techniques
Stress management is a critical component of reversing type 2 diabetes. Dr. Spages incorporates mind-body techniques such as:
- Stress Reduction Practices: Techniques like meditation, yoga, and deep-breathing exercises can lower stress hormones that negatively impact blood sugar levels.
- Sleep Optimization: Ensuring adequate and quality sleep to regulate hormones and improve insulin sensitivity.
Advanced Lifestyle Interventions
Dr. Spages advocates for a holistic lifestyle approach that includes:
- Customized Exercise Plans: Tailoring physical activity programs to individual fitness levels and preferences to ensure adherence and effectiveness.
- Behavioral Coaching: Providing support and coaching to help individuals make sustainable lifestyle changes and overcome barriers.
- Continuous Monitoring: Using technology to monitor blood sugar levels and other health metrics in real time, allowing for timely adjustments to the intervention plan.
Community and Support
Engaging with a community of like-minded individuals can provide motivation and accountability. Dr. Spages emphasizes:
- Support Groups: Participating in support groups where individuals can share experiences, challenges, and successes.
- Educational Workshops: Offering workshops and seminars to educate patients about diabetes management and reversal strategies.
Can Type 2 Diabetes Be Reversed Permanently?
The concept of permanent reversal is complex and varies among individuals. For some, maintaining remission is possible with sustained lifestyle changes and weight management. However, the risk of relapse remains, particularly if old habits are resumed. Long-term success depends on:
- Sustained Lifestyle Changes: Continued adherence to a healthy diet and regular physical activity is crucial.
- Regular Monitoring: Ongoing monitoring of blood sugar levels and medical check-ups are necessary to catch any signs of relapse early.
- Support Systems: Engaging with healthcare professionals, support groups, and family can provide the necessary encouragement and accountability.
Conclusion
While the term “reverse” might be ambitious, there is substantial evidence that type 2 diabetes can be brought into remission through significant lifestyle changes, weight management, and, in some cases, medical or surgical interventions. Achieving and maintaining remission requires a comprehensive, individualized approach and a commitment to long-term lifestyle changes. As our understanding of diabetes improves and new treatments emerge, the potential for reversing type 2 diabetes becomes increasingly attainable.
By focusing on healthy eating, regular physical activity, and weight management, many individuals with type 2 diabetes can achieve significant improvements in their health and potentially live free from the symptoms and complications of diabetes. Dr. Jonathan Spages’ advanced strategies offer a natural, drug-free approach to defying the odds and reversing type 2 diabetes, empowering patients to take control of their health and well-being.